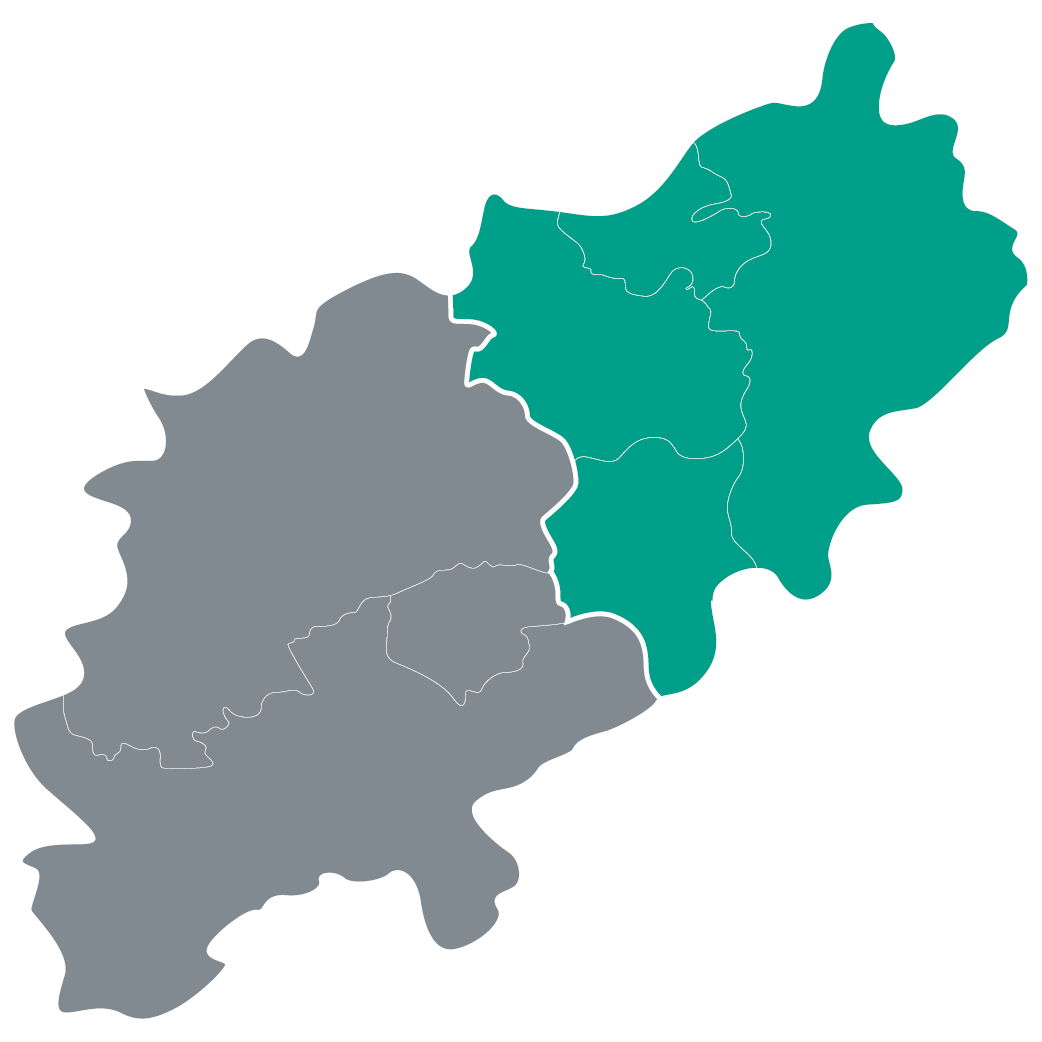
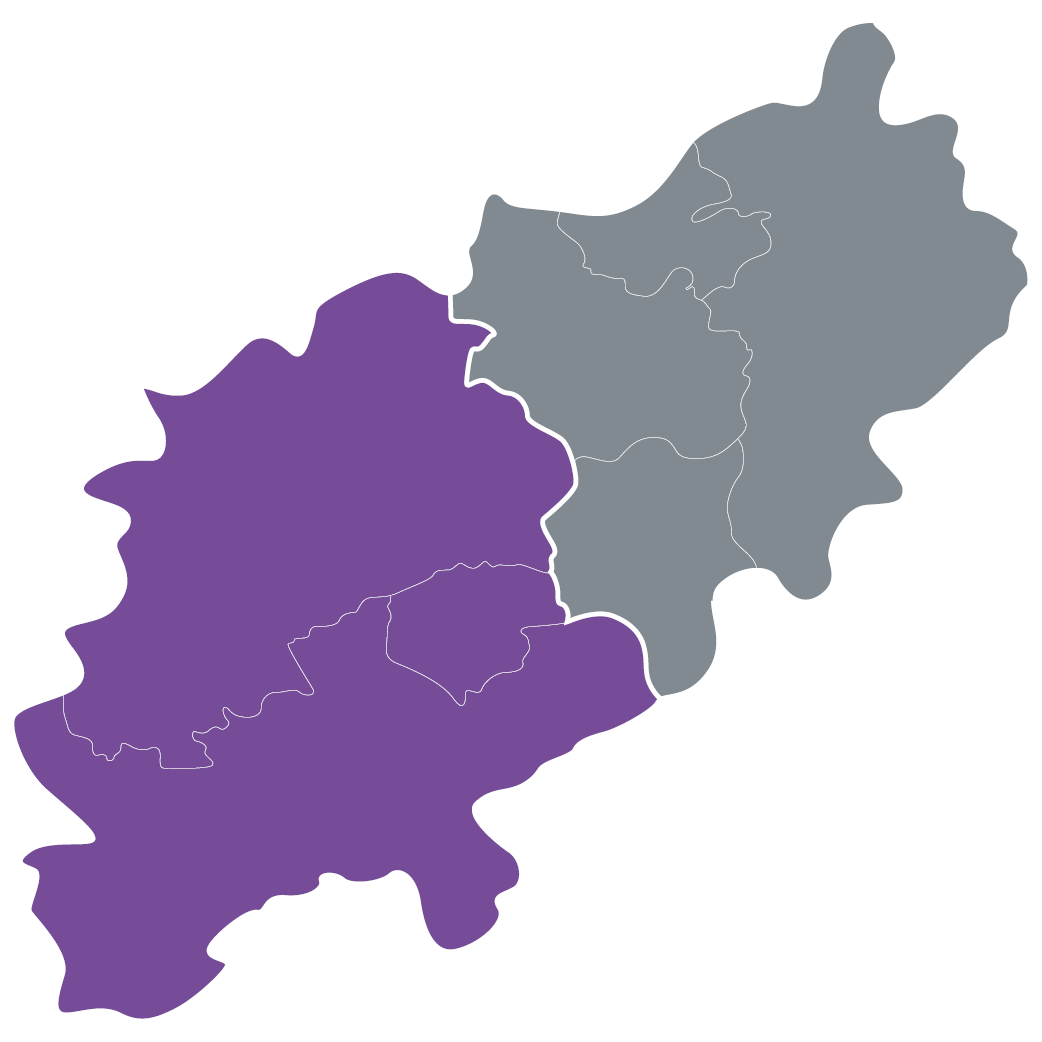
Community healthcare services (adults)
- Admiral Nursing Service
- Adult Community Hospital Inpatient Beds
- Adults Speech & Language Therapy Services
- Community Brain Injury
- Continence Service
- Community Nursing
- Community Therapy Service
- Diabetic Eye Screening Programme
- Diabetes and High Risk Foot Service
- Diabetes Northamptonshire
- Dietetics and Nutrition
- MSK Occupational Therapy Hand Therapy
- MSK Physiotherapy
- Podiatric Surgery
- Specialist Dental Services - Adult
- Post-COVID-19 and Post-Viral Rehabilitation Service
- Specialist Nursing - Heart Failure Nurse
- Specialist Nursing - Multiple Sclerosis
- Specialist Nursing - Tissue Viability
- Sexual health and HIV services
- Specialist Nursing - Parkinson’s Disease
- Specialist Palliative Care
- TB Nursing Service
- Unplanned Intermediate Care Team (ICT)